Gluten intolerance and celiac disease are increasingly recognized as significant health concerns in modern society. While both conditions involve adverse reactions to gluten—a protein found in wheat, barley, and rye—they differ in severity and underlying mechanisms. Understanding these conditions, their causes, and ways to manage them can greatly improve quality of life for those affected.
What Are Gluten Intolerance and Celiac Disease?
- Gluten Intolerance: Also known as non-celiac gluten sensitivity (NCGS), it refers to a condition where individuals experience symptoms similar to celiac disease but without the autoimmune or allergic response.
- Celiac Disease: A serious autoimmune disorder where ingestion of gluten triggers an immune response, leading to damage in the small intestine. Over time, this damage affects nutrient absorption and can lead to severe health complications if untreated.
Causes and Origins of Gluten-Related Disorders
The exact causes of gluten intolerance and celiac disease are complex and involve genetic, environmental, and lifestyle factors:
- Genetics:
- Celiac disease has a strong genetic link. Most individuals with the condition carry HLA-DQ2 or HLA-DQ8 genes, though not everyone with these genes develops the disease.
- Genetic predisposition may also play a role in gluten intolerance, although this connection is less understood.
- Autoimmune Mechanisms (Celiac Disease):
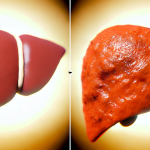
- In celiac disease, gluten ingestion causes the immune system to attack the lining of the small intestine, damaging its villi—tiny structures that absorb nutrients. This leads to malnutrition and other health problems.
- Environmental Triggers:
- Factors such as early exposure to gluten, infections, gut microbiome imbalances, and stress may increase the risk of developing gluten-related disorders.
- For celiac disease, certain events (e.g., pregnancy, surgery, or severe illness) can trigger the onset of symptoms in genetically predisposed individuals.
- Sensitivity Mechanisms (Gluten Intolerance):
- The precise cause of gluten intolerance is unclear, but it does not involve the immune system attacking the intestine as in celiac disease. Instead, it may involve the gut-brain axis or low-grade inflammation.
Symptoms of Gluten Intolerance and Celiac Disease
The symptoms of these conditions can vary widely and may overlap, making diagnosis challenging. Here’s a breakdown of common symptoms:
- Digestive Symptoms:
- Bloating, gas, and abdominal pain.
- Chronic diarrhea or constipation.
- Nausea and vomiting.
- Systemic Symptoms:
- Fatigue and brain fog.
- Headaches or migraines.
- Joint pain and muscle cramps.
- Specific to Celiac Disease:
- Unexplained weight loss or malnutrition.
- Iron-deficiency anemia not responding to treatment.
- Dermatitis herpetiformis—a blistering skin rash linked to gluten consumption.
- Long-Term Complications of Untreated Celiac Disease:
- Osteoporosis or bone weakness due to poor calcium absorption.
- Infertility and miscarriage.
- Increased risk of certain cancers, such as small bowel lymphoma.
How to Prevent Gluten-Related Disorders
While it’s not possible to prevent celiac disease in genetically predisposed individuals, certain steps may help reduce risks or manage symptoms effectively:
- Early Dietary Choices:
- Some research suggests introducing gluten to infants between 4-6 months may lower the risk of developing celiac disease. However, this should be done under medical guidance.
- Healthy Gut Maintenance:
- A balanced diet rich in fiber, prebiotics, and probiotics can support gut health and potentially reduce gluten sensitivity.
- Avoid Triggers:
- For those with celiac disease or confirmed gluten intolerance, complete avoidance of gluten is the only way to prevent symptoms and long-term complications.
Managing and Improving Life with Gluten-Related Disorders
- Gluten-Free Diet:
- The cornerstone of treatment for both gluten intolerance and celiac disease is a strict gluten-free diet. This involves avoiding all foods containing wheat, barley, rye, and their derivatives.
- Naturally gluten-free foods include fruits, vegetables, meat, fish, dairy, and gluten-free grains like rice, quinoa, and millet.
- Careful label reading is essential to avoid hidden gluten in processed foods, sauces, and seasonings.
- Regular Monitoring (Celiac Disease):
- Regular follow-ups with a healthcare provider are essential for celiac patients to monitor nutrient levels and check for complications.
- Blood tests to monitor antibodies and intestinal healing may be recommended.
- Nutritional Support:
- Nutritional deficiencies (e.g., iron, calcium, vitamin D, and B12) are common in untreated celiac disease. Supplements may be necessary during the recovery phase.
- Lifestyle Adjustments:
- Dining out can be challenging for those on a gluten-free diet. Planning ahead and communicating dietary restrictions clearly to restaurants can help.
- Emotional support through counseling or support groups can be beneficial, especially for newly diagnosed individuals.
- Medications and Emerging Therapies:
- While no medications currently cure celiac disease, ongoing research is exploring enzyme supplements and immune-modulating therapies to complement a gluten-free diet.
Conclusion
Gluten intolerance and celiac disease can significantly impact daily life, but with proper diagnosis, dietary changes, and medical support, individuals can manage these conditions effectively. Raising awareness about gluten-related disorders and their symptoms is crucial for early diagnosis and prevention of complications. By adopting a gluten-free lifestyle and staying informed, those affected can lead healthy, fulfilling lives.
For those experiencing symptoms of gluten sensitivity, consulting a healthcare professional is the first step toward finding relief and improving overall well-being.