Osteoarthritis is a chronic degenerative joint disease in which cartilage tissue deteriorates, leading to pain, stiffness, and limited mobility. The disease can affect various joints, such as the knees, hips, spine, and hands, and often develops with age. Understanding the causes of osteoarthritis can aid in prevention and slowing the progression of the disease.
Main Causes and Risk Factors for Osteoarthritis
- Age
Age is one of the main risk factors for osteoarthritis. As people age, joint cartilage wears down, and the natural regeneration process becomes less effective. The likelihood of developing osteoarthritis increases significantly in people over 50.
- Genetic Predisposition
Genetic predisposition plays an important role in the development of osteoarthritis. If close relatives (parents, siblings) have had the disease, the likelihood of its occurrence increases. Genetic factors may affect the structure of cartilage and joints, making them more vulnerable to damage.
- Excess Weight
Excess weight puts increased strain on joints, especially the knees and hips. Extra weight creates additional pressure on the cartilage, accelerating its wear. Studies show that weight loss can reduce the risk of osteoarthritis and alleviate symptoms in people who are overweight.
- Joint Injuries
Joint injuries (fractures, dislocations, sprains) increase the risk of osteoarthritis. A damaged joint may not heal properly, leading to structural abnormalities and accelerating cartilage wear. Osteoarthritis often develops in joints that have been injured or undergone surgery.
- Occupational Stress
Certain professions involve high joint strain, which increases the risk of osteoarthritis. Occupational stress on the joints is common among people whose work requires frequent bending, lifting, or prolonged standing. This creates conditions for gradual joint wear and the onset of inflammation.
- Inflammatory Processes
Chronic inflammatory processes in the joints can also contribute to osteoarthritis. Inflammation causes damage to cartilage tissue and speeds up its degradation. For example, people with rheumatoid arthritis may have an increased risk of osteoarthritis due to joint inflammation.
- Metabolic Disorders
Metabolic disorders can negatively impact joints and cartilage, promoting wear. For instance, diabetes increases the risk of osteoarthritis due to impaired blood supply and slowed tissue healing. Metabolic diseases can also cause harmful substances to accumulate, worsening joint health.
Conclusion
Causes of osteoarthritis include age, genetic predisposition, excess weight, injuries, occupational stress, inflammation, and metabolic disorders. Understanding these factors helps in preventing osteoarthritis and may slow its progression. Maintaining a healthy weight, avoiding injuries, and managing inflammatory conditions promote joint health and reduce the risk of osteoarthritis. It’s also important to seek medical help at the first signs of the disease to choose an appropriate treatment.
Osteoarthritis: Causes, Symptoms, Treatment, and Prevention
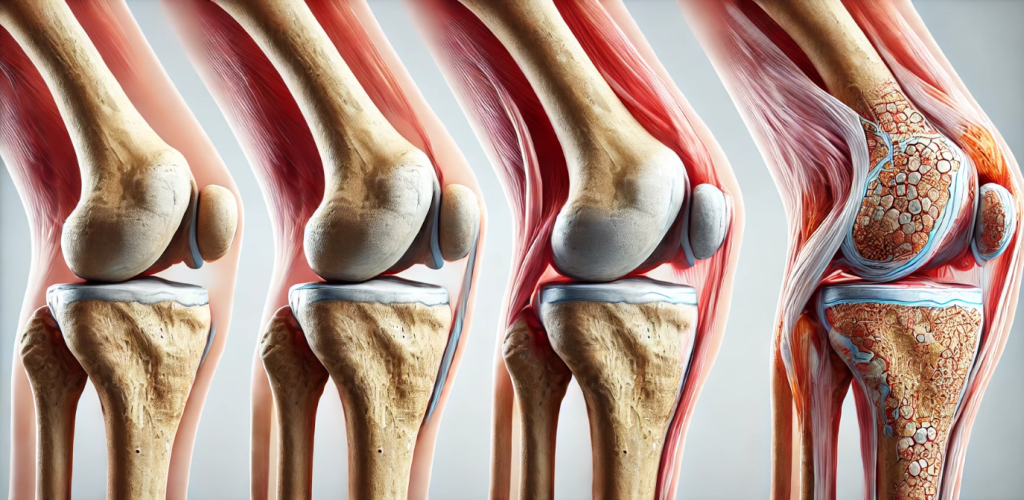
Osteoarthritis (OA) is a chronic degenerative joint disease that primarily affects the cartilage, the protective tissue at the ends of bones within joints. As the cartilage deteriorates, bones may begin to rub against each other, causing pain, stiffness, and reduced mobility. Osteoarthritis is one of the most common types of arthritis, affecting millions worldwide, particularly older adults. Understanding the causes, symptoms, and treatment options is essential for managing this condition effectively and maintaining joint health.
What Causes Osteoarthritis?
Osteoarthritis develops due to the breakdown of cartilage, which can result from a combination of factors:
- Aging:
- The risk of OA increases with age as cartilage naturally wears down over time.
- Joint Overuse:
- Repetitive stress from work, sports, or other activities can damage cartilage.
- Obesity:
- Excess body weight puts additional stress on weight-bearing joints, such as knees and hips.
- Joint Injuries:
- Previous injuries, such as fractures or ligament tears, can lead to joint instability and accelerate cartilage degeneration.
- Genetics:
- Family history of OA increases susceptibility due to inherited cartilage structure or joint shape.
- Abnormal Joint Alignment:
- Misaligned joints or congenital defects can increase pressure on specific areas of the joint.
- Other Conditions:
- Diseases such as rheumatoid arthritis or gout can contribute to the development of OA.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis vary in severity and typically develop gradually:
- Joint Pain:
- Aches or sharp pain in affected joints, especially during or after movement.
- Stiffness:
- Joint stiffness is most noticeable after waking up or periods of inactivity.
- Swelling:
- Inflammation may cause visible swelling around the joint.
- Reduced Range of Motion:
- Difficulty moving the joint fully due to pain or structural changes.
- Joint Deformity:
- In advanced stages, joints may become visibly deformed.
- Grating Sensation:
- A feeling or sound of bones grinding during movement, known as crepitus.
Weight-bearing joints such as the knees, hips, and spine are most commonly affected, though OA can also impact fingers and toes.
Diagnosing Osteoarthritis
Osteoarthritis is diagnosed through a combination of:
- Medical History and Physical Examination:
- Assessment of symptoms, joint function, and lifestyle factors.
- Imaging Tests:
- X-rays: Reveal cartilage loss, bone spurs, and joint narrowing.
- MRI: Provides detailed images of soft tissues, including cartilage and ligaments.
- Lab Tests:
- Blood tests or joint fluid analysis may be used to rule out other types of arthritis, such as rheumatoid arthritis or infection.
Treatment Options for Osteoarthritis
Treatment focuses on relieving symptoms, improving joint function, and slowing disease progression. Common approaches include:
- Lifestyle Modifications:
- Weight Management: Reducing body weight decreases stress on joints.
- Low-Impact Exercises: Activities like swimming, walking, or cycling improve joint flexibility and strengthen muscles.
- Physical Therapy:
- Tailored exercise programs help improve strength and mobility while reducing pain.
- Medications:
- Pain Relievers: Over-the-counter NSAIDs (e.g., ibuprofen, naproxen) or acetaminophen relieve pain and inflammation.
- Topical Treatments: Creams containing capsaicin or diclofenac provide localized relief.
- Injections: Corticosteroid or hyaluronic acid injections reduce inflammation and improve joint lubrication.
- Assistive Devices:
- Braces, canes, or shoe inserts help reduce pressure on affected joints.
- Surgical Intervention (Severe Cases):
- Arthroscopy: Minimally invasive procedure to remove damaged tissue.
- Joint Replacement: Total or partial replacement of severely damaged joints, commonly performed on knees or hips.
Managing Osteoarthritis Pain
Effective pain management strategies include:
- Heat and Cold Therapy:
- Apply heat to reduce stiffness and cold to alleviate swelling.
- Lifestyle Adjustments:
- Modify daily activities to avoid excessive stress on joints.
- Relaxation Techniques:
- Practices like yoga or meditation help manage pain and reduce stress.
- Supplements (with medical advice):
- Glucosamine and chondroitin are sometimes used to support joint health.
Preventing Osteoarthritis
While some risk factors for OA cannot be changed, preventive measures can significantly reduce the likelihood of developing the condition:
- Maintain a Healthy Weight:
- Reducing weight lessens the strain on weight-bearing joints.
- Stay Physically Active:
- Regular exercise strengthens muscles, supports joint stability, and improves flexibility.
- Avoid Joint Injuries:
- Use proper techniques during physical activities and sports to prevent joint damage.
- Protect Joints:
- Use appropriate ergonomic tools and supports for work or hobbies that involve repetitive motions.
- Healthy Diet:
- A balanced diet rich in antioxidants, omega-3 fatty acids, and vitamins supports joint and cartilage health.
When to Seek Medical Attention
Consult a healthcare provider if:
- You experience persistent joint pain or stiffness that interferes with daily activities.
- Swelling, redness, or warmth occurs around the joint.
- Mobility significantly decreases or joint deformity develops.
Conclusion
Osteoarthritis is a progressive condition that requires active management to maintain quality of life. Early diagnosis, combined with a holistic treatment plan, can alleviate symptoms and slow disease progression. By adopting healthy lifestyle habits and working closely with healthcare professionals, individuals with osteoarthritis can effectively manage their condition and maintain joint function.