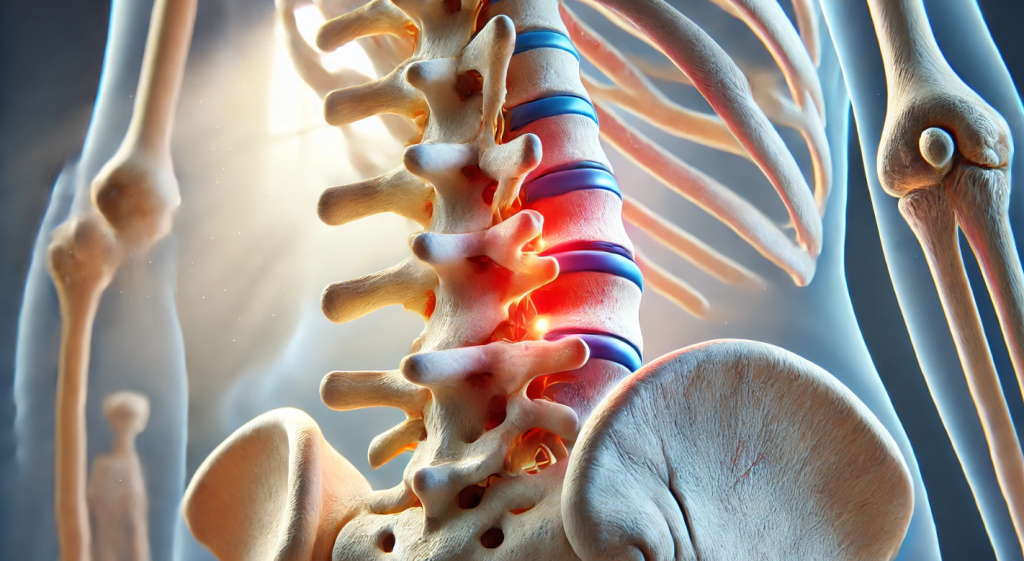
Osteochondrosis is a degenerative spinal condition that leads to the breakdown of intervertebral discs and joints. Symptoms include pain, limited mobility, and discomfort, which can significantly affect quality of life. Below are the main treatment methods for osteochondrosis to alleviate symptoms and slow disease progression.
Medications

- Pain Relievers
Analgesics or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or diclofenac are prescribed to reduce pain. - Muscle Relaxants
Muscle relaxants help relieve muscle spasms often associated with osteochondrosis. - Chondroprotectors
Drugs containing glucosamine and chondroitin promote cartilage repair and slow its degradation. - B Vitamins
B Vitamins (B1, B6, B12) improve nerve conduction and reduce neurological symptoms.
Physiotherapy
- Laser Therapy
Used to reduce inflammation and stimulate tissue regeneration. - Magnetotherapy
Improves blood circulation and alleviates pain. - Electrophoresis
With electrophoresis, medications are delivered directly to the affected areas, enhancing their effectiveness.
Therapeutic Exercises (TE)
Exercises for osteochondrosis strengthen back muscles, improve blood flow, and reduce spinal stress. Regular training helps restore mobility and prevent complications.
Manual Therapy and Massage
- Massage
Professional massage relieves muscle tension and improves blood flow. - Manual Therapy
Manual therapy sessions correct vertebral misalignments and enhance their functionality.
Orthopedic Treatment
Using specialized mattresses, pillows, and braces helps maintain the spine in the correct position, reducing strain and pain.
Lifestyle Adjustments
- Nutrition
A diet rich in calcium, magnesium, and vitamins helps strengthen bones and cartilage. - Weight Management
Excess weight increases spinal stress; weight loss positively impacts the patient’s condition. - Posture Correction
Maintaining proper posture reduces the risk of further spinal damage.
Alternative Methods

- Acupuncture
Stimulates blood circulation and relieves pain. - Apitherapy (bee venom treatment)
Reduces inflammation and improves overall well-being.
Specialist Consultation
If symptoms of osteochondrosis progress or do not respond to treatment, consult an orthopedic doctor or neurologist. A specialist will create an individualized treatment plan and recommend additional diagnostic procedures if needed.
Treating osteochondrosis requires a comprehensive approach, including medications, physiotherapy, exercises, and lifestyle changes. Timely therapy helps avoid complications and maintain quality of life.
Osteochondrosis: Causes, Symptoms, Treatment, and Prevention
Osteochondrosis is a degenerative condition of the spine caused by the gradual deterioration of intervertebral discs and surrounding tissues. This condition often affects the cervical, thoracic, or lumbar regions of the spine, leading to pain, stiffness, and reduced mobility. Osteochondrosis is commonly associated with aging, but younger individuals may also develop it due to poor posture, sedentary lifestyles, or physical trauma. Recognizing the symptoms and understanding treatment options are crucial for managing this condition effectively and preventing complications.
What Causes Osteochondrosis?
The development of osteochondrosis is influenced by several factors that contribute to the degeneration of spinal structures:
- Age-Related Changes:
- Natural wear and tear on intervertebral discs as the body ages leads to reduced elasticity and cushioning.
- Poor Posture:
- Prolonged sitting or standing in incorrect positions strains the spine and accelerates degeneration.
- Sedentary Lifestyle:
- Lack of physical activity weakens spinal muscles and reduces blood flow to discs.
- Physical Trauma:
- Injuries from accidents, heavy lifting, or repetitive strain can damage spinal structures.
- Genetic Factors:
- A family history of spinal disorders may increase susceptibility.
- Other Contributing Factors:
- Obesity, smoking, and poor nutrition can exacerbate spinal degeneration.
Symptoms of Osteochondrosis
The symptoms of osteochondrosis vary depending on the affected region of the spine:
- Cervical Osteochondrosis:
- Pain in the neck and shoulders.
- Headaches, often radiating from the back of the head.
- Dizziness and impaired coordination.
- Numbness or tingling in the arms or hands.
- Thoracic Osteochondrosis:
- Pain in the mid-back or chest, sometimes mistaken for heart conditions.
- Stiffness and discomfort during deep breathing or twisting movements.
- Lumbar Osteochondrosis:
- Lower back pain that may radiate to the hips, thighs, or legs.
- Muscle weakness or numbness in the lower extremities.
- Difficulty bending, lifting, or prolonged sitting.
Severe cases can lead to complications such as herniated discs, nerve compression, or spinal deformities.
Diagnosing Osteochondrosis
A healthcare provider will use a combination of methods to diagnose osteochondrosis:
- Medical History and Physical Examination:
- Evaluating symptoms, lifestyle, and family history.
- Imaging Studies:
- X-rays, MRI, or CT scans provide detailed views of the spine, revealing disc degeneration, bone spurs, or herniations.
- Neurological Assessments:
- Tests to evaluate nerve function, reflexes, and muscle strength, especially if nerve compression is suspected.
Treatment Options for Osteochondrosis
Treatment focuses on alleviating symptoms, improving spinal function, and preventing further degeneration. Options include:
- Medications:
- Pain Relievers: Over-the-counter NSAIDs (e.g., ibuprofen, naproxen) reduce pain and inflammation.
- Muscle Relaxants: Relieve muscle spasms and stiffness.
- Topical Analgesics: Creams or gels for localized pain relief.
- Prescribed Medications: In severe cases, corticosteroids or stronger pain medications may be used.
- Physical Therapy:
- Exercises to strengthen spinal muscles, improve flexibility, and restore posture.
- Techniques such as traction, massage, and electrotherapy for pain relief.
- Lifestyle Modifications:
- Adopting an ergonomic workspace to reduce strain on the spine.
- Maintaining a healthy weight to reduce pressure on intervertebral discs.
- Incorporating regular low-impact exercises like swimming or walking.
- Chiropractic Care:
- Manual adjustments to improve spinal alignment and mobility.
- Alternative Therapies:
- Acupuncture, yoga, or Pilates may complement traditional treatments.
- Surgical Intervention (Rare):
- Reserved for cases involving severe nerve compression, spinal instability, or unmanageable pain.
- Procedures may include discectomy, laminectomy, or spinal fusion.
Preventing Osteochondrosis
Preventive measures can significantly reduce the risk of developing osteochondrosis or slow its progression:
- Maintain Good Posture:
- Practice proper sitting, standing, and lifting techniques to minimize strain on the spine.
- Stay Active:
- Regular exercise strengthens spinal muscles and promotes flexibility.
- Healthy Lifestyle Choices:
- Eat a balanced diet rich in calcium, vitamin D, and other nutrients essential for bone health.
- Avoid smoking, which impairs disc nutrition and healing.
- Ergonomic Adjustments:
- Use supportive chairs, proper desk height, and appropriate footwear.
- Regular Check-Ups:
- Early detection of spinal issues through routine medical evaluations can prevent complications.
When to Seek Medical Attention
Consult a healthcare provider if you experience:
- Persistent or worsening pain that interferes with daily activities.
- Numbness, tingling, or weakness in the limbs.
- Difficulty controlling bladder or bowel movements (a potential sign of a medical emergency, such as cauda equina syndrome).
Conclusion
Osteochondrosis is a manageable condition with timely intervention and consistent care. Recognizing early symptoms and adopting a proactive approach to treatment can significantly improve quality of life and prevent complications. Regular exercise, lifestyle modifications, and professional medical support are essential for maintaining spinal health and overall well-being.














Pingback: 7 Main Causes of Back Pain: Identifying the Source of Discomfort - Medhouse.info