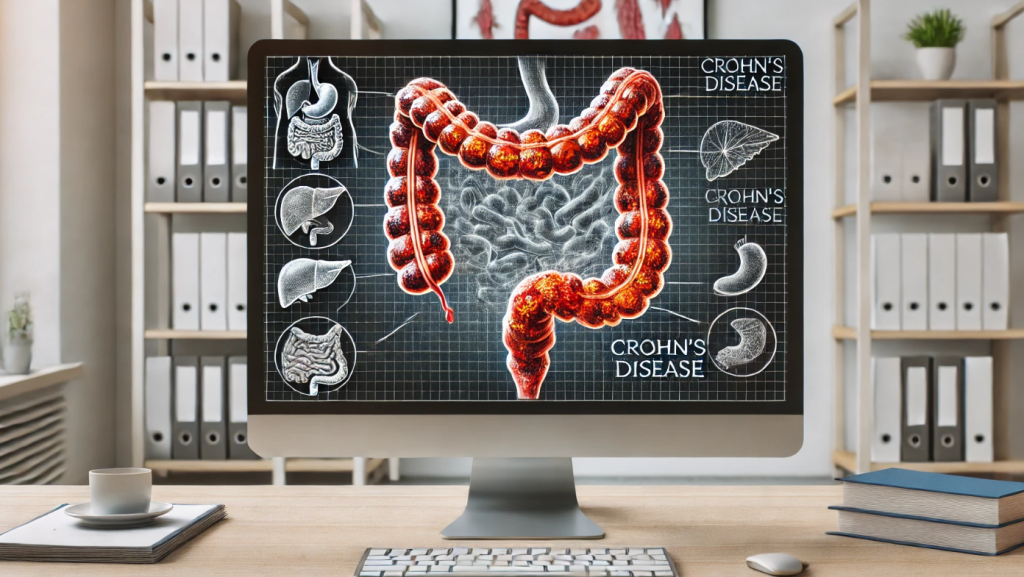
Crohn’s disease is a chronic inflammatory condition of the gastrointestinal tract that can affect any part, from the mouth to the anus. It often leads to severe complications, impacting quality of life. Recognizing the symptoms of Crohn’s disease early helps initiate treatment and prevent complications.
Key Symptoms

- Abdominal Pain
One of the most common symptoms is cramping pain in the abdomen, especially in the lower right quadrant. This is due to inflammation and narrowing of the intestines. - Diarrhea
Diarrhea in Crohn’s disease is often chronic, sometimes containing mucus or blood. It is caused by intestinal inflammation and impaired water absorption. - Weight Loss
Loss of appetite and malabsorption of nutrients lead to significant weight loss in patients. - Fatigue and Weakness
Chronic inflammation results in constant fatigue and a sense of low energy. - Blood in Stool
The presence of blood indicates damage to the intestinal lining caused by inflammation. - Fever
An elevated body temperature indicates active inflammation in the body. - Skin, Eye, and Joint Changes
Some patients experience extraintestinal manifestations, such as arthritis, uveitis, and skin rashes.
Complications
- Bowel Obstruction
Narrowing of the intestinal lumen due to inflammation or scarring. - Fistulas and Abscesses
Formation of abnormal channels between the intestine and other organs. - Nutritional Deficiencies
Impaired absorption of vitamins and minerals, especially B12, iron, and calcium.
When to See a Doctor?

- If you have chronic diarrhea, abdominal pain, or blood in your stool.
- If you notice significant weight loss or persistent fatigue.
- If you have a family history of inflammatory bowel disease.
Diagnosis and Treatment
Diagnosis of Crohn’s disease includes endoscopic examinations (colonoscopy), blood and stool tests, and imaging methods like MRI and CT scans. Treatment may involve anti-inflammatory drugs, immunomodulators, biologic therapy, and, in severe cases, surgery.
Crohn’s Disease: Causes, Symptoms, Treatment, and Management
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. It most commonly impacts the end of the small intestine (ileum) and the beginning of the large intestine (colon). The disease causes inflammation that can lead to pain, diarrhea, and other severe complications. According to statistics, Crohn’s disease affects approximately 3 million adults in the United States and millions more globally. While the exact cause is not fully understood, advances in treatment and management have significantly improved quality of life for those living with this condition.
What Causes Crohn’s Disease?
The exact cause of Crohn’s disease remains unclear, but researchers believe it results from a combination of factors:
- Genetics: Individuals with a family history of Crohn’s disease are at a higher risk, with up to 20% of patients having a close relative with IBD.
- Immune System Dysfunction: An overactive immune response may attack the GI tract, causing chronic inflammation.
- Environmental Factors: Certain environmental triggers, such as infections, smoking, or a high-fat diet, may initiate or worsen the condition.
- Gut Microbiota Imbalance: Changes in the gut bacteria composition may contribute to disease progression.
Crohn’s disease is more commonly diagnosed in individuals between the ages of 15 and 35, though it can occur at any age. Smoking and living in urban, industrialized areas have also been identified as risk factors.
Symptoms of Crohn’s Disease
The symptoms of Crohn’s disease vary depending on the severity and location of inflammation in the GI tract. Common symptoms include:
- Persistent diarrhea, often with urgency.
- Abdominal pain and cramping, particularly in the lower right abdomen.
- Blood in the stool.
- Weight loss and malnutrition due to poor absorption of nutrients.
- Fatigue and general weakness.
- Fever during flare-ups.
In more severe cases, Crohn’s disease can lead to complications such as intestinal strictures (narrowing of the bowel), fistulas (abnormal connections between organs), or abscesses. Extraintestinal symptoms, like joint pain, skin conditions, or eye inflammation, may also occur.
Diagnosing Crohn’s Disease
Diagnosing Crohn’s disease typically involves a combination of tests and evaluations:
- Medical History and Physical Examination: Symptoms, family history, and lifestyle factors are reviewed.
- Blood Tests: These identify signs of inflammation, infection, or anemia.
- Stool Tests: Help rule out infections and detect markers of intestinal inflammation.
- Endoscopy and Colonoscopy: Visualize inflammation and take biopsies of affected areas in the GI tract.
- Imaging Tests: MRI or CT scans assess the extent of inflammation and complications like fistulas or abscesses.
Accurate diagnosis is essential for distinguishing Crohn’s disease from other IBDs, such as ulcerative colitis, and tailoring an effective treatment plan.
Treatment Options for Crohn’s Disease
While there is no cure for Crohn’s disease, treatment focuses on reducing inflammation, managing symptoms, and preventing complications. Common treatment approaches include:
- Medications:
- Anti-inflammatory Drugs: Corticosteroids, such as prednisone, can reduce inflammation during flare-ups.
- Immune Modulators: Medications like azathioprine suppress the immune response to prevent ongoing inflammation.
- Biologic Therapies: Anti-TNF agents like infliximab or adalimumab target specific pathways in the immune system to control symptoms.
- Antibiotics: Used to treat or prevent infections in the GI tract.
- Dietary Adjustments:
- While no specific diet cures Crohn’s disease, avoiding trigger foods like spicy dishes, dairy, or high-fiber items can reduce symptoms.
- Nutritional supplements or liquid diets may be necessary to address malnutrition.
- Surgery:
- In cases where medications are ineffective or complications like strictures or fistulas arise, surgery may be required. Procedures may include removing damaged sections of the intestine or repairing fistulas.
- Lifestyle Changes:
- Quitting smoking is critical, as it exacerbates symptoms and increases the risk of complications.
- Stress management techniques, such as yoga or mindfulness, can improve quality of life.
Managing Crohn’s Disease
Living with Crohn’s disease requires a proactive approach to managing symptoms and maintaining remission. Regular check-ups with a gastroenterologist ensure that treatments remain effective. Tracking symptoms and potential triggers can help identify patterns and adjust care accordingly.
Staying physically active and maintaining a balanced diet tailored to individual needs supports overall health. Community support groups and mental health counseling are invaluable for coping with the emotional challenges of a chronic illness.
Current Advances in Crohn’s Disease Research
Ongoing research continues to explore new treatment options for Crohn’s disease. Innovations such as personalized medicine, gut microbiota transplants, and advanced biologics show promise in achieving better outcomes for patients. Studies also focus on understanding the role of genetics and environmental factors in disease progression.
When to Seek Medical Attention
It is important to consult a healthcare provider if symptoms like persistent diarrhea, severe abdominal pain, or unintentional weight loss occur. Signs of complications, such as fever, blood in the stool, or difficulty eating, require urgent evaluation.
Conclusion
Crohn’s disease is a challenging but manageable condition with the right treatment and lifestyle adjustments. Early diagnosis, personalized care, and advances in medical research provide hope for improving the quality of life for those living with this chronic illness. By understanding the condition and working closely with healthcare providers, individuals with Crohn’s disease can achieve long-term remission and lead fulfilling lives.