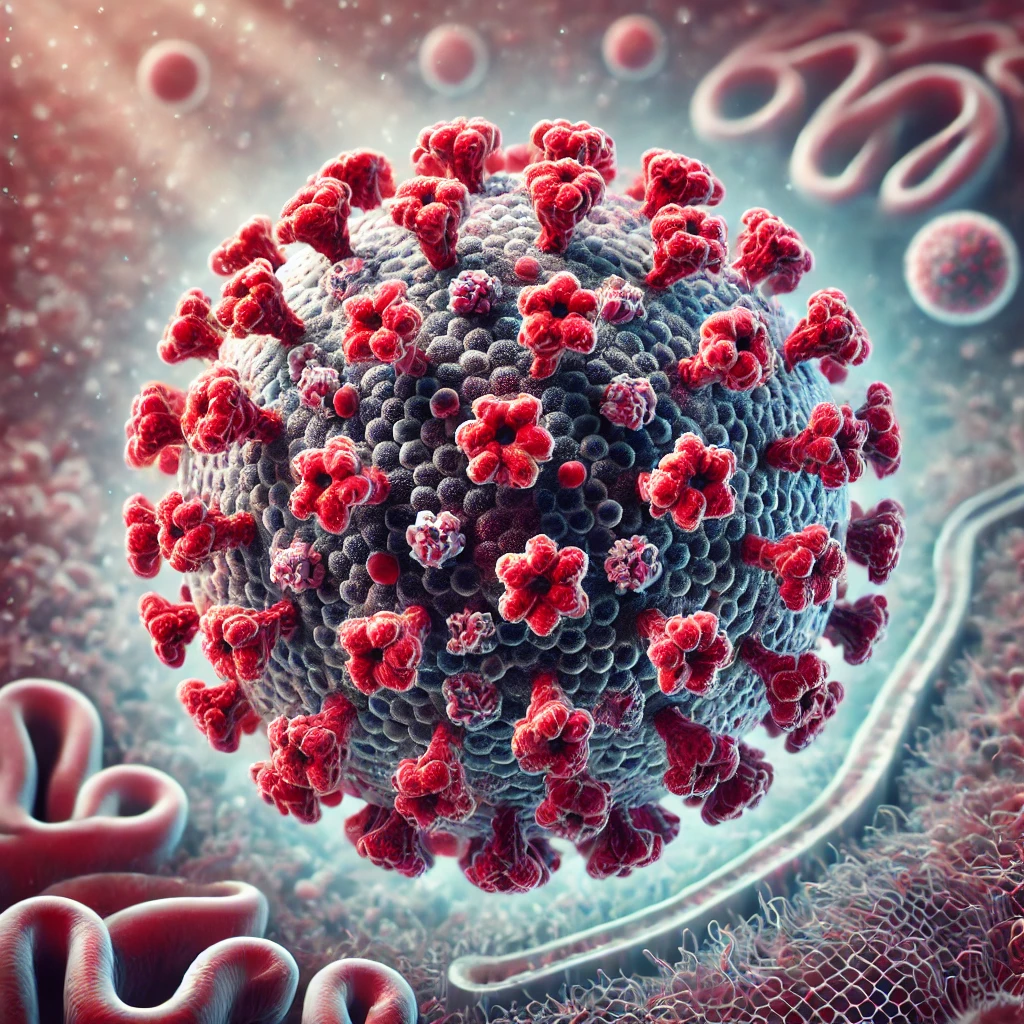
Human Metapneumovirus (HMPV) is a common respiratory virus that affects people of all ages, especially young children, older adults, and individuals with weakened immune systems. Although HMPV Virus often causes mild cold-like symptoms, it can lead to more severe illnesses, such as bronchitis and pneumonia. This article explores the symptoms, transmission, diagnosis, treatment, and prevention of HMPV in a clear and simple way.
What is HMPV?
Imagine waking up with a stuffy nose, a scratchy throat, and a cough that just won’t go away. You might think it’s just a common cold or maybe the flu. But what if it’s something else—something most people haven’t even heard of? Meet Human Metapneumovirus, or HMPV, a sneaky respiratory virus that’s been quietly making people sick for decades. While it often causes mild symptoms, it can sometimes lead to more serious illnesses, especially in young children, older adults, and those with weakened immune systems. In this article, we’ll explore everything you need to know about HMPV—from its history to its symptoms, treatments, and prevention tips—so you can feel prepared and informed.
HMPV, or Human Metapneumovirus has been circulating for decades. It belongs to the Paramyxoviridae family, the same group of viruses that includes measles and mumps. HMPV primarily targets the respiratory system, causing infections that range from mild to severe.
Discovery and History of HMPV
HMPV was first identified in 2001 by Dutch researchers who isolated the virus from respiratory tract samples of children with unexplained respiratory infections. Genetic analysis revealed that HMPV belonged to the Paramyxoviridae family, closely related to the avian metapneumovirus, indicating its evolutionary origins. Retrospective studies found evidence of HMPV circulating in human populations for over 50 years, despite its recent identification. Researchers believe that advances in molecular techniques allowed for its discovery, as it had previously been misclassified under other respiratory illnesses.

Symptoms of HMPV
HMPV symptoms are often similar to those of other respiratory illnesses, such as the flu or the common cold. However, the severity and progression can vary depending on age, overall health, and immune function.
Common Symptoms:
- Runny nose and nasal congestion
- Persistent cough, which may worsen at night
- Sore throat or scratchiness
- Mild to moderate fever
- Sneezing and watery eyes
- Fatigue and body aches
Severe Symptoms:
In more serious cases, particularly in high-risk groups, symptoms can escalate to:
- Shortness of breath or labored breathing (dyspnea)
- Wheezing or tightness in the chest
- High fever that persists for several days
- Bluish skin (cyanosis) due to low oxygen levels
- Severe dehydration, indicated by dry mouth, reduced urination, or dizziness
Sensory and Physical Experiences:
Patients often report:
- A heavy sensation in the chest, making it difficult to take deep breaths.
- Sharp or dull chest pain when coughing.
- Muscle weakness or exhaustion, even after mild activity.
- Chills and shivering, accompanied by sweating.
- A dry, tickling sensation in the throat leading to persistent coughing fits.
Infants and toddlers may display:
- Irritability or difficulty feeding.
- Rapid breathing or nasal flaring.
- Grunting noises during breathing.
How is HMPV Virus Transmitted?
HMPV spreads through respiratory droplets, similar to other respiratory viruses. Common methods of transmission include:
- Close contact with an infected person
- Inhalation of droplets released through coughing or sneezing
- Touching contaminated surfaces and then touching the face (mouth, nose, or eyes)
Because HMPV can survive on surfaces for several hours, maintaining proper hygiene is critical in preventing its spread.
How to Share With Just FriendsHow to share with just friends.
Posted by Facebook on Friday, December 5, 2014
Who is at Risk?
While anyone can get HMPV, certain groups are more vulnerable:
- Infants and Young Children: Developing immune systems make them more susceptible.
- Older Adults: Aging can weaken the immune system, increasing vulnerability.
- People with Chronic Illnesses: Conditions like asthma, COPD, or heart disease heighten the risk.
- Immunocompromised Individuals: Cancer patients, organ transplant recipients, and those with HIV are at greater risk.
Diagnosing HMPV
Doctors may suspect HMPV based on symptoms and exposure history, but a laboratory test is needed for confirmation. Diagnosis typically involves:
- Nasopharyngeal Swab: A sample is collected from the nose or throat.
- PCR Testing: Detects genetic material of the virus.
- Antigen Testing: Identifies proteins specific to HMPV.
Treatment Options
Currently, there is no specific antiviral medication for HMPV. Treatment focuses on relieving symptoms and supporting recovery:
- Rest and Hydration: Helps the body fight the infection naturally.
- Over-the-Counter Medications: Pain relievers, such as ibuprofen or acetaminophen, reduce fever and aches.
- Cough Suppressants and Decongestants: Provide temporary relief from congestion and coughing.
- Oxygen Therapy: Severe cases may require supplemental oxygen or hospitalization.
- Nebulizers and Bronchodilators: These are sometimes used to ease breathing difficulties in severe cases.
Medications Used in Treatment:
Though no antiviral drugs specifically target HMPV, symptomatic treatment includes:
- Acetaminophen or ibuprofen for fever and pain relief.
- Antihistamines for nasal congestion.
- Bronchodilators (e.g., albuterol) for wheezing.
- Antibiotics, only if secondary bacterial infections develop.
HMPV Virus Research and Studies
Studies show that HMPV accounts for approximately 5–10% of respiratory infections globally. Research in the United States estimates that HMPV hospitalizes about 20,000–25,000 children under age 5 annually. In Europe, data suggests HMPV is responsible for 10–15% of acute respiratory infections in hospitalized children and elderly patients.
Key findings include:
- HMPV is more prevalent during the winter and early spring seasons.
- Studies suggest 20–30% of patients with severe respiratory illness test positive for HMPV.
- Ongoing vaccine research is showing promising results, with clinical trials underway to assess efficacy and safety.
HMPV Virus Prevention Tips
Preventing HMPV infection is similar to avoiding other respiratory illnesses:
- Hand Hygiene: Wash hands regularly with soap and water for at least 20 seconds.
- Avoid Close Contact: Stay away from individuals who are sick.
- Disinfect Surfaces: Clean frequently-touched areas, such as doorknobs and phones.
- Cover Coughs and Sneezes: Use a tissue or your elbow to prevent spreading germs.
- Stay Home if Sick: Limit exposure to others to avoid transmitting the virus.
Immunization:
As of now, there is no vaccine for HMPV, but researchers are working on developing one.
How Does HMPV Differ From Other Viruses?
HMPV is often mistaken for other respiratory viruses, including:
- Respiratory Syncytial Virus (RSV): Similar symptoms but different genetic makeup.
- Influenza (Flu): HMPV does not cause sudden high fever or muscle aches like the flu.
- COVID-19: Testing is needed to distinguish between HMPV and COVID-19 due to overlapping symptoms.
When to See a Doctor?
Seek medical attention if you or someone you care for experiences:
- Difficulty breathing
- Persistent high fever
- Severe dehydration (dry mouth, dizziness, or no urination)
- Worsening symptoms despite home care
Conclusion
Human Metapneumovirus (HMPV) is a common yet often overlooked respiratory infection. While most cases are mild and resolve on their own, high-risk groups may experience severe complications. Understanding symptoms, risk factors, and prevention methods can help reduce its impact.
By practicing good hygiene and seeking medical advice for severe cases, you can protect yourself and others from HMPV. Researchers are continuing to study the virus, with hopes of developing a vaccine in the future.